by C MICHAUDET · Cited by 36 — by asthma, protracted bacterial bronchitis, and upper airway cough syndrome. Evaluation should focus initially on these etiologies, with.
225 KB – 6 Pages
PAGE – 1 ============
November 1, 2017 ˜ Volume 96, Number 9 www.aafp.org/afp American Family Physician 575 Although chronic cough in adults (cough lasting longer than eight weeks) can be caused by many etiologies, four conditions account for most cases: upper airway cough syndrome, gastroesophageal re˜ux disease/laryngopharyn -geal re˜ux disease, asthma, and nonasthmatic eosinophilic bronchitis. Patients should be evaluated clinically (with spirometry, if indicated), and empiric treatment should be initi -ated. Other potential causes include angiotensin-converting enzyme inhibitor use, environmental triggers, tobacco use, chronic obstruc -tive pulmonary disease, and obstructive sleep apnea. Chest radiogra -phy can rule out concerning infectious, in˜ammatory, and malignant thoracic conditions. Patients with refractory chronic cough may warrant referral to a pulmonologist or otolaryngologist in addi -tion to a trial of gabapentin, pregabalin, and/or speech therapy. In children, cough is considered chronic if present for more than four weeks. In children six to 14 years of age, it is most commonly caused by asthma, protracted bacterial bronchitis, and upper airway cough syndrome. Evaluation should focus initially on these etiologies, with targeted treatment and monitoring for resolution. ( Am Fam Physi -cian . 2017;96(9): 575-580 . Copyright © 2017 American Academy of Family Physicians.) ILLUSTRATION BY JONATHAN DIMES Chronic Cough: Evaluation and Management CHARLIE MICHAUDET, MD, and JOHN MALATY, MD, University of Florida College of Medicine, Gainesville, Florida Cough caused by the common cold typically lasts one to three weeks and is self-limited . However, per -sistent chronic cough can be the ˜rst sign of a more serious disease process. According to the Centers for Disease Control and Prevention, cough of undifferentiated duration is the most common presenting symptom in patients of all ages in the primary care ambulatory setting. 1 In adults, chronic cough is de˜ned as symptoms lasting longer than eight weeks, whereas acute cough lasts less than three weeks and subacute cough from three to eight weeks. 2 When persistent and excessive, cough can seriously impair quality of life and lead to vomiting, muscle pain, rib fractures, urinary incontinence, tiredness, syncope, and depression. It also has psychosocial effects, such as embarrassment and negative impact on social interactions. 3 This article presents a systematic approach to the evaluation of chronic cough, derived from the results of prospective studies and an evidence-based practice guideline. 4,5 Assessment of Chronic Cough The initial evaluation should focus on iden -tifying potential triggers, such as the use of an angiotensin-converting enzyme (ACE) inhibitor, environmental exposures, smok -ing status, and chronic obstructive pulmo -nary disease (COPD). It should also rule out red ˚ags (e.g., fever, weight loss, hemoptysis, hoarseness, excessive dyspnea or sputum production, recurrent pneumonia, smok -ing history of 20 pack-years , or smoker older than 45 years) that suggest a serious underly -ing cause of cough. 6 The patient™s description of the cough (character, timing, presence or CME This clinical content conforms to AAFP criteria for continuing medical education (CME). See CME Quiz on page 567. Author disclosure: No rel -evant ˜nancial af˜liations. ˚ Patient information: A handout on this topic is available at http://www. aafp.org/afp/2011/1015/ p894.html .BEST PRACTICES IN PULMONARY MEDICINE: RECOMMENDATIONS FROM THE CHOOSING WISELY CAMPAIGN Recommendation Sponsoring organization Do not diagnose or manage asthma without spirometry. American Academy of Allergy, Asthma and Immunology Cough and cold medicines should not be prescribed or recommended for respiratory illnesses in children younger than four years. American Academy of Pediatrics Source: For more information on the Choosing Wisely Campaign, see http://www. choosingwisely.org . For supporting citations and to search Choosing Wisely recom -mendations relevant to primary care, see http://www.aafp.org/afp/recommendations/ search.htm .
PAGE – 2 ============
576 American Family Physician www.aafp.org/afp Volume 96, Number 9 ˜ November 1, 2017 absence of sputum production) should not determine the clinical approach; sequen -tial or concomitant treatment of common causes is still recommended. 4 Unless a likely cause is identi˜ed, chest radiography should be obtained to rule out most infectious, in˚ammatory, and malignant thoracic con -ditions. When physical examination ˜nd -ings are normal and no red ˚ags are present, routine computed tomography of the chest and sinuses is not necessary, nor is initial bronchoscopy. 2 The diagnostic approach should focus on detection and treatment of the four most common causes of chronic cough in adults: upper airway cough syndrome (UACS), asthma, nonasthmatic eosinophilic bron -chitis, and gastroesophageal re˚ux disease (GERD)/laryngopharyngeal re˚ux disease. 4,5 After evaluation and empiric management of these etiologies, less common causes should be considered (Tables 1 7 and 2 8). A suggested primary care approach to the evaluation of chronic cough for immunocompetent adults is shown in Figure 1 .9Common Causes of Chronic Cough UPPER AIRWAY COUGH SYNDROME The term UACS, previously referred to as postnasal drip syndrome, was coined in the 2006 American College of Chest Phy -sicians guideline 4 in recognition of the fact that multiple etiologies, including chronic rhinosinusitis, allergic rhinitis, and SORT: KEY RECOMMENDATIONS FOR PRACTICE Clinical recommendation Evidence rating References In adults with chronic cough, initial evaluation should focus on the most common causes: upper airway cough syndrome, gastroesophageal or laryngopharyngeal re˜ux disease, asthma, and nonasthmatic eosinophilic bronchitis. Other causes to consider include angiotensin-converting enzyme inhibitor use, environmental triggers, tobacco use, and chronic obstructive pulmonary disease. C2, 4-6, 10, 14, 20- 22, 24, 26, 30, 35 In patients with refractory chronic cough, referral to a pulmonologist or otolaryngologist should be considered, as well as a trial of gabapentin (Neurontin), pregabalin (Lyrica), or speech therapy. C4, 5, 36, 38-41 In children six to 14 years of age with chronic cough, initial evaluation should focus on the most common causes: asthma, protracted bacterial bronchitis, and upper airway cough syndrome. C4, 6, 42-44 A = consistent, good-quality patient-oriented evidence; B = inconsistent or limited-quality patient-oriented evidence; C = consensus, disease-oriented evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, go to http://www.aafp.org/afpsort. Table 1. Etiologies of Chronic Cough in Adults and Children Adults Most common Angiotensin-converting enzyme inhibitor use Asthma Environmental triggers Gastroesophageal/laryngopharyngeal re˜ux disease Nonasthmatic eosinophilic bronchitis Tobacco use Upper airway cough syndrome Less common Bronchiectasis Chronic obstructive pulmonary disease Obstructive sleep apnea Pertussis Postinfectious bronchospasm Least common Arteriovenous malformation Bronchiolitis Bronchogenic carcinoma Chronic aspiration Chronic interstitial lung disease Irritation of external auditory canal Persistent pneumonia Psychogenic cough Sarcoidosis Tuberculosis Children Most common Asthma Protracted bacterial bronchitis Upper airway cough syndrome (in children older than six years) Less common Environmental triggers Foreign body (in younger children) Gastroesophageal re˜ux disease Pertussis Postinfectious bronchospasm Least common Chronic aspiration Congenital abnormality Cystic ˚brosis Immunode˚ciency Primary ciliary dyskinesia Psychogenic cough Tourette syndrome/tic Adapted with permission from Benich JJ III, Carek PJ. Evaluation of the patient with chronic cough. Am Fam Physician . 2011;84(8):888.
PAGE – 3 ============
November 1, 2017 ˜ Volume 96, Number 9 www.aafp.org/afp American Family Physician 577 nonallergic rhinitis, were dif˜cult to differentiate solely by clinical presentation. UACS is the most common cause of chronic cough. 10 Rhinorrhea, nasal stuf˜ness, sneezing, itching, and postnasal drainage suggest the diagnosis, but their absence does not rule out UACS. 11 Physical ˜ndings may include swollen turbinates and direct visualization of postnasal drainage and cobble -stoning of the posterior pharynx. If a speci˜c cause is identi˜ed, therapy should be started; otherwise, initial treatment includes a decongestant combined with a ˜rst-generation antihistamine. Intranasal corticoste -roids, saline nasal rinses, nasal anticholinergics, and antihistamines are also reasonable options. 10 Clinical improvement should occur within days to weeks, and up to two months. If chronic rhinosinusitis is sus -pected, sinus computed tomography or ˚exible naso -laryngoscopy should be performed. Sinus radiography is not recommended because of limited sensitivity. 12ASTHMA AND COPD The prevalence of asthma in patients with chronic cough ranges from 24% to 29%. 13 It should be suspected in patients with shortness of breath, wheezing, and chest tightness, but cough can be the only manifestation in cough variant asthma. If the physical examination and spirometry ˜ndings are nondiagnostic, bronchial chal -lenge testing (methacholine inhalation test) should be considered. 14 Resolution of the cough after asthma treat -ment is also diagnostic. After counseling the patient about potential triggers, treatment usually includes an inhaled bronchodilator and high-dose inhaled corticosteroid. A leukotriene receptor antagonist (e.g., montelukast [Sin -gulair]) can also be useful. Symptoms should resolve within one to two weeks after starting treatment. 15-17 For severe or refractory cough, a ˜ve- to 10-day course of prednisone, 40 to 60 mg, or equivalent oral corticosteroid can be considered if asthma is strongly suspected. 4,13 COPD commonly causes chronic cough, but most patients presenting with chronic cough do not have undiagnosed COPD. Signs and symptoms suggestive of asthma also occur in persons with COPD. Spirom -etry is diagnostic, and purulent sputum production may also be present. Treatment includes an inhaled bronchodilator, inhaled anticholinergic, inhaled corticosteroid, and a one- to two-week course of oral corticoste -roids (with or without antibiotics). 18NONASTHMATIC EOSINOPHILIC BRONCHITIS Nonasthmatic eosinophilic bronchitis is characterized by chronic cough in patients with no symptoms or objective evidence of variable air˚ow obstruction, normal airway responsiveness on a methacholine inhala -tion test, and sputum eosinophilia. 19 Sputum evaluation is not typically performed in the primary care setting, but it can be induced by saline nebulization or obtained by bron -choalveolar lavage in a subspecialist™s of˜ce. The prevalence is unclear, but studies assess -ing airway in˚ammation in patients with chronic cough showed that this condition accounts for 10% to 30% of cases referred for subspecialist investigation. 14,20 It does not respond to inhaled bronchodilators, but should respond to inhaled corticoste -roids. Avoidance strategies should be recom -mended when the in˚ammation is due to occupational exposure or inhaled allergens. Table 2. Abnormalities That Suggest Speci˜c Etiologies of Cough Abnormality Suggested etiology Auscultatory ˚ndings Wheeze: intrathoracic airway lesions (e.g., asthma, tracheomalacia) Crepitations: airway lesions (from secretions) or parenchymal disease (e.g., interstitial disease) Cardiac abnormalities Associated airway abnormalities, cardiac failure Chest pain Arrhythmia, asthma Chest wall deformity Pulmonary airway or parenchymal disease Daily moist or productive cough Suppurative lung disease Digital clubbing Suppurative lung disease Dyspnea or tachypnea Pulmonary airway or parenchymal disease Exertional dyspnea Pulmonary airway or parenchymal disease Failure to thrive Serious systemic illness (including pulmonary illness, such as cystic ˚brosis) Feeding dif˚culties Aspiration, serious systemic illness (including pulmonary illness) Hemoptysis Suppurative lung disease, vascular abnormalities Hypoxia/cyanosis Pulmonary airway or parenchymal disease, cardiac disease Immunode˚ciency Atypical infection, suppurative lung disease Neurodevelopmental abnormality Aspiration lung disease Recurrent pneumonia Atypical infection, congenital lung abnormality, immunode˚ciency, suppurative lung disease, tracheoesophageal ˚stula Adapted with permission from Chang AB, Glomb WB. Guidelines for evaluating chronic cough in pediatrics: ACCP evidence-based clinical practice guidelines. Chest . 2006; 129(1 suppl): 262S.
PAGE – 4 ============
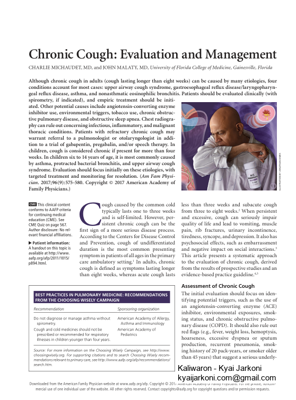
578 American Family Physician www.aafp.org/afp Volume 96, Number 9 ˜ November 1, 2017 Oral corticosteroids are rarely needed but can be consid -ered if high-dose inhaled corticosteroids are ineffective. 14GASTROESOPHAGEAL/LARYNGOPHARYNGEAL REFLUX DISEASE The prevalence of GERD and laryngopharyngeal re˚ux disease as causative factors in chronic cough varies from 0% to 73%. 21 Studies have shown an association between GERD and chronic cough, but the pathophysiology is complex and treatment is controversial. 2,22,23 Associ -ated manifestations such as heartburn, regurgitation, sour taste, hoarseness, and globus sensation are clini -cal clues. Although several uncontrolled studies have shown improvement of chronic cough with antacid treatment, more recent randomized controlled trials have shown no differences between proton pump inhibi -tors and placebo. 24-29 Although there is poor evidence that proton pump inhibitors are universally bene˜cial for GERD-induced chronic cough, 30 consensus guide -lines recommend empiric therapy for at least eight weeks in conjunction with lifestyle changes such as dietary changes and weight loss. 4,31 The addition of a histamine H2 receptor antagonist and/or baclofen (Lioresal, 20 mg per day) may be helpful. 32,33 A link between obstructive sleep apnea and chronic cough has been investigated. Treatment with continu -ous positive airway pressure may improve chronic cough by decreasing GERD; therefore, evaluation for obstruc -tive sleep apnea should be considered. 34 Surgery can be considered in patients with GERD-associated chronic cough who have abnormal esophageal acid exposure (as proven by pH testing) if normal peristalsis is con˜rmed on manometry. 31ACE InhibitorŒRelated Cough ACE inhibitorŒrelated cough has been reported in 5% to 35% of patients and is more common in women. 35 It may start within hours to months of the ˜rst dose. When the medication is discontinued, resolution of the cough should occur within one week to three months; this is the only way to determine if the ACE inhibitor is causing the cough. Angiotensin receptor blockers are a good alternative to ACE inhibitors. However, if the patient has a strong indi -cation, restarting the ACE inhibitor may be attempted; in some patients, the cough will not recur. 35 When con -sidering ACE inhibitors as the cause of chronic cough, other common causes should also be investigated. Options for Refractory Cough Patients with unexplained chronic cough after evaluation and treatment of common causes should be referred to a pulmonologist or otolaryngologist. 4,5 Neuromodulators have shown some bene˜t in randomized trials based on the hypothesis that refractory chronic cough may be due to hypersensitivity of the cough re˚ex caused by peripheral (afferent limb of the cough re˚ex) and central mechanisms Evaluation of Chronic Cough in Adults Figure 1. Algorithm for assessment of chronic cough in immunocompetent adults. (GERD = gastroesophageal re˜ux disease.) Adapted with permission from Iyer VN, Lim KG. Chronic cough: an update. Mayo Clin Proc . 2013;88(10):1118. Chronic cough > 8 weeks Evaluate for red ˜ags Consider chest radiography Exclude: Angiotensin-converting enzyme inhibitor use Environmental exposures Smoking Chronic obstructive pulmonary disease Potential cause identi˚ed? Treat speci˜c cause Upper airway cough syndrome GERD/laryngopharyngeal re˜ux disease Asthma Nonasthmatic eosinophilic bronchitis Other identi˚ed cause (Table 1) Sequential or concomitant empiric treatment Upper airway cough syndrome GERD/laryngopharyngeal re˜ux disease Asthma Nonasthmatic eosinophilic bronchitis If symptoms continue Refractory chronic cough Consider: Referral to pulmonologist/otolaryngologist Further testing (e.g., chest computed tomography, bronchoscopy, obstructive sleep apnea screening) Gabapentin (Neurontin)/pregabalin (Lyrica)/speech therapy If symptoms continue NoYes
PAGE – 5 ============
November 1, 2017 ˜ Volume 96, Number 9 www.aafp.org/afp American Family Physician 579(central sensitization). 36-38 Therapies included gabapentin (Neurontin, 1,800 mg per day), which improved symp -toms within four weeks; pregabalin (Lyrica, 300 mg per day) in conjunction with speech therapy, which showed greater improvement vs. placebo with speech therapy; and speech and language therapy alone. 39-41 Chronic Cough in Children Chronic cough in children younger than 15 years is de˜ned as cough lasting more than four weeks. 8 Chest radiography and spirometry should be considered ini -tially in age-appropriate patients. 8 A watch-wait -review approach consisting of parental reassurance and obser -vation for one to two weeks may be used in patients with a nonspeci˜c cough. 8,42 The most common causes of chronic cough in chil -dren six to 14 years of age are asthma, protracted bac -terial bronchitis, and UACS. 4,6,42 Protracted bacterial bronchitis is characterized by isolated chronic cough, wet/moist cough, resolution of cough with antibiotic treatment, and absence of ˜ndings suggestive of an alter -native cause. Treatment consists of a two-week course of an appropriate antibiotic, such as amoxicillin/clavula -nate (Augmentin). 43,44 UACS is rare in children younger than six years, and antihistamines and decongestants are not recom -mended. 44 GERD does not seem to be as common in children, and empiric proton pump inhibitors are not recommended in the absence of a speci˜c diagnosis. 8 Exposure to tobacco smoke, pets, and environmental irritants should be minimized. Pertussis can be consid -ered but is usually associated with other symptoms, such as a fiwhoopfl sound, apnea, low-grade fever, or vomit -ing. Less common causes, such as foreign body aspira -tion, congenital conditions, cystic ˜brosis, and immune disorders, should also be considered. This article updates previous articles on this topic by Benich and Carek, 7 Holmes and Fadden, 45 and Lawler. 46Data Sources: A PubMed search was conducted combining the key term cough with chronic, adults, children, causes, etiologies, evaluation, treatment, asthma, re˚ux, upper airway cough syndrome, postnasal drip, and non-asthmatic eosinophilic bronchitis. In addition, searches were conducted using these terms on the Agency for Healthcare Research and Quality website, the National Guideline Clearinghouse database, Essential Evidence Plus, Clinical Evidence, and the Cochrane Database of Systematic Reviews. Search dates: August 5, 2016, to March 6, 2017. The Authors CHARLIE MICHAUDET, MD, is an assistant professor in the Community Health and Family Medicine Department at the University of Florida Col -lege of Medicine, Gainesville. JOHN MALATY, MD, is an associate professor in the Community Health and Family Medicine Department at the University of Florida College of Medicine. Address correspondence to John Malaty, MD, University of Florida College of Medicine, 1707 N. Main St., Gainesville, FL 32609 ( e-mail : malaty@u˜.edu ). Reprints are not available from the authors. REFERENCES 1. Centers for Disease Control and Prevention. National ambulatory medi -cal care survey: 2013 state and national summary tables. https: //www. cdc.gov/nchs/data/ahcd/namcs_summary/2013_namcs_web_tables.pdf . Accessed August 28, 2017. 2. Irwin RS, Madison JM. The diagnosis and treatment of cough. N Engl J Med . 2000; 343(23): 1715-1721 . 3. French CL, Irwin RS, Curley FJ, Krikorian CJ. Impact of chronic cough on quality of life. Arch Intern Med . 1998; 158(15): 1657-1661 . 4. Irwin RS, Baumann MH, Bolser DC, et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest . 2006; 129(1 suppl): 1S-23S . 5. Irwin RS, French CT, Lewis SZ, Diekemper RL, Gold PM; CHEST Expert Cough Panel. Overview of the management of cough: CHEST guideline and expert panel report. Chest . 2014; 146(4): 885-889 . 6. Gibson PG, Chang AB, Glasgow NJ, et al. CICADA: cough in children and adults: diagnosis and assessment. Australian cough guidelines sum -mary statement. Med J Aust . 2010; 192(5): 265-271 . 7. Benich JJ III, Carek PJ. Evaluation of the patient with chronic cough. Am Fam Physician. 2011; 84(8): 887-892 . 8. Chang AB, Glomb WB. Guidelines for evaluating chronic cough in pedi -atrics: ACCP evidence-based clinical practice guidelines. Chest . 2006; 129(1 suppl): 260S-283S . 9. Iyer VN, Lim KG. Chronic cough: an update. Mayo Clin Proc . 2013; 88 (10): 1115-1126 . 10. Pratter MR. Chronic upper airway cough syndrome secondary to rhino -sinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest . 2006; 129(1 suppl): 63S-71S . 11. Mello CJ, Irwin RS, Curley FJ. Predictive values of the character, timing, and complications of chronic cough in diagnosing its cause. Arch Intern Med . 1996; 156(9): 997-1003 . 12. Meltzer EO, Hamilos DL, Hadley JA, et al.; American Academy of Allergy, Asthma and Immunology (AAAAI); American Academy of Otolaryngic Allergy (AAOA); American Academy of OtolaryngologyŠ Head and Neck Surgery ( AAO-HNS ); American College of Allergy, Asthma and Immunology (ACAAI); American Rhinologic Society (ARS). Rhinosinusitis: establishing de˚nitions for clinical research and patient care. J Allergy Clin Immunol . 2004; 114(6 suppl): 155-212 . 13. Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest . 2006; 129(1 suppl): 75S-79S . 14. Brightling CE. Cough due to asthma and nonasthmatic eosinophilic bronchitis. Lung . 2010; 188(suppl 1): S13-S17 . 15. Irwin RS, French CT, Smyrnios NA, Curley FJ. Interpretation of positive results of a methacholine inhalation challenge and 1 week of inhaled bronchodilator use in diagnosing and treating cough-variant asthma. Arch Intern Med . 1997; 157(17): 1981-1987 . 16. Johnstone KJ, Chang AB, Fong KM, Bowman RV, Yang IA. Inhaled cor -ticosteroids for subacute and chronic cough in adults. Cochrane Data -base Syst Rev . 2013; (3): CD009305. 17. Ribeiro M, Pereira CA, Nery LE, Beppu OS, Silva CO. High-dose inhaled beclomethasone treatment in patients with chronic cough: a random -ized placebo-controlled study. Ann Allergy Asthma Immunol . 2007; 99(1): 61-68 .
PAGE – 6 ============
580 American Family Physician www.aafp.org/afp Volume 96, Number 9 ˜ November 1, 2017 18. Qureshi H, Sharafkhaneh A, Hanania NA. Chronic obstructive pulmo -nary disease exacerbations: latest evidence and clinical implications. Ther Adv Chronic Dis . 2014; 5(5): 212-227 . 19. Brightling CE, Ward R, Goh KL, Wardlaw AJ, Pavord ID. Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med . 1999; 160(2): 406-410 . 20. Da˛browska M, Grabczak EM, Arcimowicz M, et al. Causes of chronic cough in non-smoking patients. Adv Exp Med Biol . 2015; 873: 25-33 . 21. Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet . 2008; 371(9621): 1364-1374 . 22. Irwin RS, Richter JE. Gastroesophageal re˜ux and chronic cough. Am J Gastroenterol . 2000; 95(8 suppl): S9-S14 . 23. Kahrilas PJ, Smith JA, Dicpinigaitis PV. A causal relationship between cough and gastroesophageal re˜ux disease (GERD) has been estab -lished: a pro/con debate. Lung . 2014; 192(1): 39-46 . 24. Irwin RS, Corrao WM, Pratter MR. Chronic persistent cough in the adult: the spectrum and frequency of causes and successful outcome of spe -ci˚c therapy. Am Rev Respir Dis . 1981; 123(4 pt 1): 413-417 . 25. Irwin RS, Zawacki JK, Curley FJ, French CL, Hoffman PJ. Chronic cough as the sole presenting manifestation of gastroesophageal re˜ux. Am Rev Respir Dis . 1989; 140(5): 1294-1300 . 26. Waring JP, Lacayo L, Hunter J, Katz E, Suwak B. Chronic cough and hoarseness in patients with severe gastroesophageal re˜ux disease. Diagnosis and response to therapy. Dig Dis Sci . 1995; 40(5): 1093-1097 . 27. Faruqi S, Molyneux ID, Fathi H, Wright C, Thompson R, Morice AH. Chronic cough and esomeprazole: a double-blind placebo-controlled parallel study. Respirology . 2011; 16(7): 1150-1156 . 28. Reichel O, Dressel H, Wiederänders K, Issing WJ. Double-blind , placebo- controlled trial with esomeprazole for symptoms and signs associated with laryngopharyngeal re˜ux. Otolaryngol Head Neck Surg . 2008; 139(3): 414-420 . 29. Shaheen NJ, Crockett SD, Bright SD, et al. Randomised clinical trial: high-dose acid suppression for chronic cough – a double-blind , placebo- controlled study. Aliment Pharmacol Ther . 2011; 33(2): 225-234 . 30. Chang AB, Lasserson TJ, Gaffney J, Connor FL, Garske LA. Gastro- oesophageal re˜ux treatment for prolonged non-speci˚c cough in chil -dren and adults. Cochrane Database Syst Rev . 2011; (1): CD004823. 31. Kahrilas PJ, Altman KW, Chang AB, et al.; CHEST Expert Cough Panel. Chronic cough due to gastroesophageal re˜ux in adults: CHEST guide -line and expert panel report. Chest . 2016; 150(6): 1341-1360 . 32. Dicpinigaitis PV, Dobkin JB. Antitussive effect of the GABA-agonist baclofen. Chest . 1997; 111(4): 996-999 . 33. Xu X, Lv H, Yu L, Chen Q, Liang S, Qiu Z. A stepwise protocol for the treatment of refractory gastroesophageal re˜ux-induced chronic cough. J Thorac Dis . 2016; 8(1): 178-185 . 34. Sundar KM, Daly SE. Chronic cough and OSA: an underappreciated rela -tionship. Lung . 2014; 192(1): 21-25 . 35. Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough: ACCP evidence-based clinical practice guidelines. Chest . 2006; 129(1 suppl): 169S-173S . 36. Morice AH, Millqvist E, Belvisi MG, et al. Expert opinion on the cough hypersensitivity syndrome in respiratory medicine. Eur Respir J . 2014; 44(5): 1132-1148 . 37. Haque RA, Usmani OS, Barnes PJ. Chronic idiopathic cough: a discrete clinical entity? Chest . 2005; 127(5): 1710-1713 . 38. Driessen AK, McGovern AE, Narula M, et al. Central mechanisms of air -way sensation and cough hypersensitivity. Pulm Pharmacol Ther . 2017: S1094-S5539 (17) 30016-0 . 39. Ryan NM, Birring SS, Gibson PG. Gabapentin for refractory chronic cough: a randomised, double-blind , placebo-controlled trial. Lancet . 2012; 380(9853): 1583-1589 . 40. Vertigan AE, Kapela SL, Ryan NM, Birring SS, McElduff P, Gibson PG. Pregabalin and speech pathology combination therapy for refractory chronic cough: a randomized controlled trial. Chest . 2016; 149(3): 639-648 . 41. Chamberlain Mitchell SA, Garrod R, Clark L, et al. Physiotherapy, and speech and language therapy intervention for patients with refractory chronic cough: a multicentre randomised control trial. Thorax . 2017; 72(2): 129-136 . 42. Asilsoy S, Bayram E, Agin H, et al. Evaluation of chronic cough in chil -dren. Chest . 2008; 134(6): 1122-1128 . 43. Chang AB, Upham JW, Masters IB, et al. Protracted bacterial bronchi -tis: the last decade and the road ahead. Pediatr Pulmonol . 2016; 51(3): 225-242 . 44. Marchant J, Masters IB, Champion A, Petsky H, Chang AB. Randomised controlled trial of amoxycillin clavulanate in children with chronic wet cough. Thorax . 2012; 67(8): 689-693 . 45. Holmes RL, Fadden CT. Evaluation of the patient with chronic cough. Am Fam Physician . 2004; 69(9): 2159-2166 . 46. Lawler WR. An of˚ce approach to the diagnosis of chronic cough. Am Fam Physician. 1998; 58(9): 2015-2022 .
225 KB – 6 Pages